MSGM Case Presentation July 2025
- Malaysian Society of Geriatric Medicine
- Jul 1, 2025
- 4 min read
Updated: Jul 7, 2025
Title: Atypical Dementia: A Puzzle in Motion
Prepared by : Dr Nuur Habibah Ghazali
Supervised by: Dr Tan IJ, Dr Alan Pok
Location: Hospital Kuala Lumpur
Madam V is a 79-year-old Indian lady with a history of hypertension, dyslipidaemia, and lacunar stroke with no residual weakness.
Presenting illness
In May 2024, this patient presented with a 3-week history of lethargy and reduced oral intake, accompanied by noticeable changes in behaviour. She became verbally and physically aggressive, exhibited shouting and hitting behaviour with psychotic features, including both auditory and visual hallucinations. There were no signs or symptoms indicative of ongoing infection; she did not experience fever, cough, abdominal discomfort, or gastrointestinal loss.
Upon initial assessment, the patient was found to be confused and disoriented to time, person, and place. Clinical examination revealed signs of dehydration. Neurologically, she exhibited a fine resting tremor in her left hand, but there were no signs of rigidity or bradykinesia. Motor strength in both upper and lower limbs was at least 3/5 bilaterally. No focal neurological deficits were observed.
Her psychiatric history includes a diagnosis of Major Depressive Disorder with psychotic features, established approximately one year ago. She was previously managed with Sertraline 50mg once daily and Risperidone 1mg nightly under psychiatric care in Sungai Petani, Kedah.
However, following a recent relocation to Kuala Lumpur one month ago, the family planned to transition the psychiatry care to HKL. Unfortunately, due to a motor vehicle accident involving her granddaughter, the patient missed her scheduled psychiatric follow-up and has been non-compliant with both Sertraline and Risperidone for the past month.
Given her clinical presentation and history of medication non-adherence, the psychiatry team reviewed her during admission. They concluded that she was experiencing a relapse of depression with psychosis, likely triggered by the abrupt discontinuation of her antidepressant and antipsychotic medications. She was restarted on Risperidone 0.5mg nightly as part of her management plan.
Chronological History of Events (2023 – Mid-2024)
Cognition and Behaviour/Mood
The patient began exhibiting mild cognitive impairment around the year 2020, at the age of 75. This included forgetfulness of recent events, difficulty recalling conversations, and frequently misplacing items. The onset was subtle and gradual, with symptoms remaining relatively stable over the years and not causing significant concern to the patient or her family.
However, throughout 2023, there was a marked decline in her mental state, primarily with the emergence of psychotic symptoms. She experienced vivid auditory hallucinations, often involving conversations with deceased relatives such as her husband and son. Some of these voices issued dangerous commands, including instructions to remove her clothes or jump off the balcony. Additionally, she reported intermittent visual hallucinations of “ghosts,” especially in the evenings, which led her to avoid certain rooms out of fear. These were accompanied by persecutory delusions, particularly the belief that her daughter and son-in- law were trying to harm her using black magic.
Significant behavioural disturbances accompanied these psychotic features. The patient became increasingly agitated, often verbally abusive, and occasionally physically aggressive, such as throwing objects at her daughter during confrontations. Her affect also changed; she appeared more withdrawn, exhibited sadness, had difficulty sleeping, and was noted to wander at night.
In February 2023, these psychiatric symptoms culminated in an impulsive ingestion of Clorox, prompting emergency medical intervention. A CT brain scan at that time revealed multifocal infarcts, leading to a working diagnosis of possible vascular dementia with Behavioural and Psychological Symptoms of Dementia (BPSD). She was discharged with Risperidone 0.5mg BD, but subsequently defaulted on her psychiatric follow-up.
From mid-2023 to mid-2024, her psychiatric condition continued to fluctuate. Although her memory impairment remained stable, her hallucinations, delusions, low mood, and aggressive behaviour persisted.
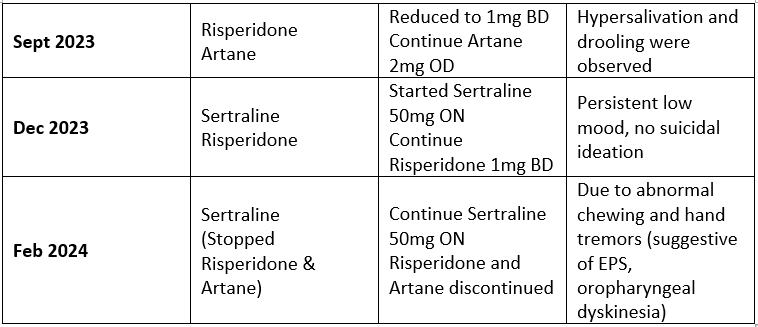
Medication history

Functional status summary

Progress during admission
On Day 5 of admission, after two days of initiating Risperidone, the patient was observed to have developed a pill-rolling tremor of her left hand.
Questions:
1. The patient's cognitive decline began with subtle forgetfulness in 2020, remaining relatively stable until more prominent neuropsychiatric features emerged in 2023. Given this trajectory, what is the possible underlying pathology and neurocognitive diagnosis?
2. How do the prominent neuropsychiatric symptoms and the presence of extrapyramidal signs influence your diagnosis?
MMSE:


Question:
3. How does the additional information from the MMSE and CT brain findings impact your working diagnosis?
A clinical conundrum
Given the diagnostic complexity of Madam V's case, characterised by psychotic symptoms of visual and auditory hallucinations, low mood, Parkinsonism with antipsychotics, and fluctuating cognition, the team encountered challenges in distinguishing between Lewy Body Dementia, depression with psychosis, and vascular cognitive impairment. Although the clinical features do suggest probable LBD, the presence of multifocal infarcts on CT and overlapping features necessitated additional neuroimaging to confirm the diagnosis and guide management decisions.
Therefore, an FDG-PET scan was arranged to assess for patterns of cortical hypometabolism characteristic of neurodegenerative dementias.

Questions:
4. Would the additional information from the PET scan change the pharmacological intervention, particularly regarding the use of antipsychotics or cholinesterase inhibitors?
5. Should this patient be followed primarily under geriatrics, neurology, or psychiatry, and what multidisciplinary supports would you involve?

Comments