MSGM Case Presentation October 2024
- Malaysian Society of Geriatric Medicine
- Oct 1, 2024
- 4 min read
Prepared by Ting Lee Yee
Supervised by Prof Terence Ong
Title When Two Worlds Collide: MRSA Bacteraemia and Parkinson's Complexity
Mr K was a 70-year-old, married, nursing home (NH) resident , with the following comorbidities:
Parkinson’s disease (PD) with camptocormia, dementia with behavioural and
psychological symptoms (BPSD)
Hypertension
History of posterior circulation infarct with basilar artery thrombosis 1.5 years ago with no residual weakness
Benign thyroid cyst
Medications reviews as follows:
T. Madopar 125mg BD
T. Piribedil 50mg BD
T. Selegilline 10mg OM
T. Quetiapine 150mg ON
T. Exforge (Amlodipine 10/ Valsartan 80) 1⁄2 tab OD
Not on aspirin / statin
He was admitted to University Hospital on 7/6/2024 presenting with 1 week history of fever with documented temperature of 38°C, partially relieved with paracetamol associated with poor oral intake and slight concentrated urine. Otherwise, other systematic review was unremarkable. Collateral history obtained from wife suggested that his food intake was poor made worst with underlying florid hallucination and delusion of harm (food was laced with poison or mixed with faecal and urinary matters) despite on regular dose of his antipsychotics.
Physical examination revealed a frail, mildly dehydrated, delirious ‘hunchback’ gentleman with enlarged goitre. Vital sign examinations revealed no obvious murmur, regular heart rhythm with fair pulse volume while lungs were clear and abdomen were soft, non-tender.
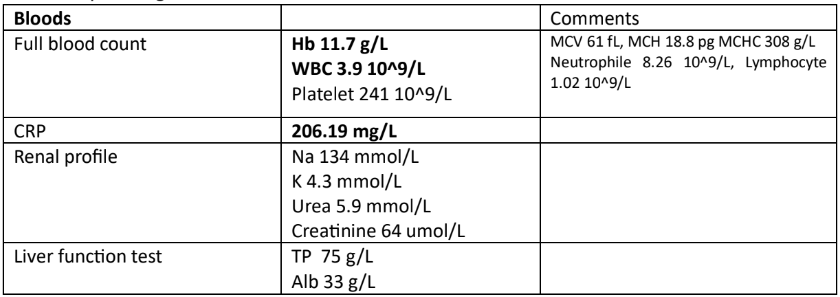
Preliminary investigations revealed:
CXR
A provisional diagnosis of occult sepsis with source likely from urinary tract was made with IV Augmentin and hydration initiated.
Additional history obtained from wife:
NH resident since January 2023 as wife, whom was the primary caretaker suffered a stroke and was unable to care for his increasing needs
o Frequent change in NH in view of unmanageable behaviours (hallucination and delusions)
o Recent NH cost RM5000/month with a room shared by two occupants
Baseline premorbid: Clinical Frailty Scale (CFS) 7
o bADL: Katz score 7, needs help with bathing and clothing, ambulating short distance with walking frame with supervision, able to self-feed but pampers-dependent for toilet needs
o iADL: Lawton score 1 (phone), rest dependent, occasionally he had the pleasure of going out to have meals with friends who came to pick him up from nursing home, or goes back home on weekend on a 2-weekly basis
Mr K had a prolonged hospital stay totalling 1 month with several issues to highlight.
Persistent methicillin resistant staphylococcus aureus (MRSA) bacteraemia
-Initial urine cultures grew Staphylococcus, however <10^4 organism/ml
-Antibiotics were escalated to IV Vancomycin when first Blood culture (peripheral vein) grew MRSA
-Co-managed with Infectious disease team
-Workup to locate source was difficult
Transthoracic echocardiogram (TTE) inpatient revealed no vegetations
No open/ chronic wound examined after wife gave skin as possible entry as
patient tend to ‘prick’ his skin to extract ‘needles’ inserted by people who
wish to harm him
No prior recent admission with history of thrombophlebitis
USG abdomen (done 3 weeks into admission) revealed no intraabdominal
collection
*Unable to proceed with CT TAP and TOE due to physical limitation (unable to lie
flat)
-Anaesthesiologist colleagues identified concerns that risks outweigh the benefits for CT scan done under sedation with muscle relaxant with ICU backup
-Radiology colleagues expressed few concerns if proceed CT scan such as
limited views with artefacts
potential injuries sustained if attempting to forcefully bend the neck to fit the
tunnel
-Slow to achieve culture clearance despite targeted antibiotic
Serial Blood CS
Blood C&S (4/6/24) - MRSA
Blood C&S (7/6/24) - MRSA
Blood C&S (10/6/24) - MRSA
Blood C&S (12/6/24) - MRSA
Blood C&S (18/6/24) - MRSA
Blood C&S (21/6/24) - MRSA
Blood C&S (23/6/24) - MRSA
Blood C&S (25/6/24) - MRSA
Blood C&S (27/6/24) – MRSA
Blood C&S (29/6/2024) – No growth
Antibiotic summary
IV Augmentin 1.2g TDS (3/6-7/6) 5 days
IV Vancomycin 800mg STAT and BD (7/6 – 24/6/2024) 18 days
IV Cefazolin 2g TDS (7/6 – 24/6/2024) 18 days
IV linezolid 600mg BD 24/6/2024 – 26/6/2024 (3 days) ID quota
IV Daptomycin 750mg OD 27/6/2024 till 30/6/2024
IV Ceftaroline 600mg TDS 27/6/2024 till 30/6/2024
Parkinson disease complexity
-diagnosed 15 years ago, starting with ambulation issues (slowness and stiffness)
-noted cognitive decline since 2020 with mild hallucination and delusions, noticeable after his covid vaccination
-BPSD worsen this year with delusions of harm, citing scams, attempted made on his life via multiple means
-physically notice progression over recent 2 years with worsening posture rendering mobility issues (he was last seen by wife able to ambulate 10 steps with support (caregiver need to position him properly and hold his walking frame) 3 weeks prior admission
-Co-managed with Neurology team for optimization of medication (increased Madopar from 175mg BD to TDS
-Inpatient therapist implied poor rehab potential
-Rehab colleagues’ impression was kyphoscoliosis of cervical and thorax, not for Botox injections as no spasticity
-Hallucination contributed to medication non-compliance as patient tend to self-adjust his own medications (Madopar deemed will make hallucination worst with intermittent dyskinesia)
Other issues to note briefly including
Mixed delirium: multifactorial (dehydration, electrolyte imbalance, underlying Parkinson’s disease with dementia
Feeding issues: oral intake was fair throughout hospitalization made worst with abnormal neck posture with risk of aspiration pneumonia, advanced directives in placed not for nasogastric tube insertion
Worsening pressure injury: From deep pressure injury to Grade 3 sacral sore
Anaemia: multifactorial including acute illness, frequent blood taking for culture clearance
Meeting patient’s and wife’s expectations
Unfortunately, Mr K desaturated on 30/6/2024 with SPO2 reading dips down to 88% under room air requiring FM02 10L/min, spiking temperature up to 38°C and found to be delirious, pulling out his condom catheter. Repeated CXR showed no consolidation. He eventually succumbed to death on 1/7/2024 as per prior established advanced directions for comfort care with cause of death given: Persistent MRSA bacteraemia.
Questions:
1. What other investigations could be done to identify the source of persistent MRSA bacteraemia? What other teams would be able to help manage his condition?
2. Should the antibiotics be escalated earlier? If so, total duration of treatment if unable to local possible source?
3. Can camptocormia be prevented or treated, as Mr K’s inability to lie flat impacted his care (investigate source of infection, pressure injury care etc)?
4. How best to manage psychosis in PD?
5. When do we decided for withdrawal therapy in this patient?



Comments